Your vaginal health is just as important pre and post menopause, but what changes should you expect?
Vaginal discharge and dryness often go hand in hand during the menopause phases of your life, with one quickly identifying if there is an issue with the other, and by now we know that decreasing oestrogen levels are the main culprit for vaginal dryness and thinning of the vaginal walls.
What no one told you was just how uncomfortable this can be if not addressed, leading to a range of symptoms, including itching, burning, and pain during intercourse.
Here is our guide on what to expect pre and post menopause, and a few tips to manage and help alleviate the symptoms.
The great news is that whilst many people see an increase in vaginal discharge during the peri-menopause phase, this reduces significantly post-menopause and as a result of decreasing oestrogen levels.
However, this can also come with it's own set of new problems as vaginal dryness becomes more common, and one of the first signs something may not be right is abnormal discharge.
Because periods can be so unpredictable during the peri-menopause with ovulation not always taking place at every cycle, your discharge will vary from month to month in both how much is produced and it's consistency, but if it's generally white, or clear in colour, it's not a cause for concern.
Post-menopause and as part of the natural aging process, discharge becomes thinner, and is white, or pale yellow in colour and this too is perfectly normal.
Sadly, as the decrease in the oestrogen hormone progresses and the vaginal lining starts to become thinner, you may find that infections start to be noticed and one of the most common signs an infection is present is abnormal discharge, especially if it's accompanied by itching, and an unpleasant odour!
Thinning vaginal tissues can lead to infections such a bacterial vaginosis, or yeast infections. Now, as unwelcome and uncomfortable as these are, they are easily treated with over the counter creams, pessaries or oral medication from your chemist.
If however, you are post-menopausal and have discharge that contains blood, or is pink and brown in colour you should book an appointment with your doctor to rule out any serious medical conditions.
You can reduce the instances of vaginal infections by practicing good intimate hygiene, avoiding fragranced toiletries and always wiping from front to back when visiting the toilet.
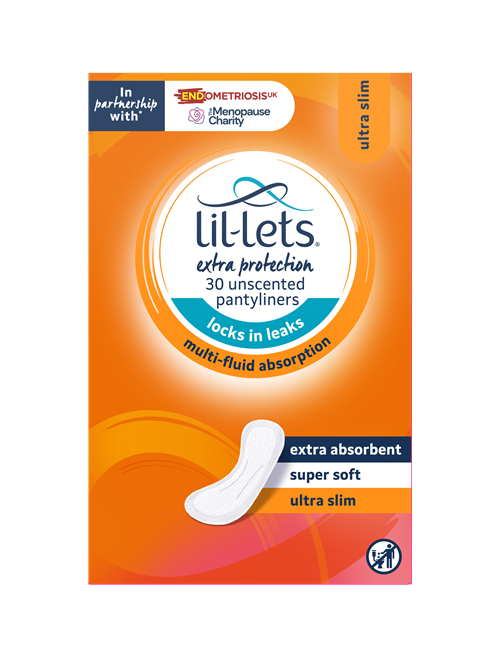
Now may also be a time to consider wearing pantyliners, especially as discharge can be so unpredictable. The Extra Protection pantyliners from Lil-Lets will not only help manage discharge, but also any unexpected bladder leaks too!
Lil-Lets Extra Protection SmartFit LinersIrritation, discomfort, vaginal infections and pain during intercourse are just a few signs that you may be suffering with vaginal dryness.
Genitourinary Syndrome of Menopause (GSM) is the term used to describe a collection of symptoms that are associated with menopause and changes to both the genital and urinary systems. Unfortunately, for those that suffer with vaginal dryness it can significantly impact their quality of life.
Oestrogen plays a crucial part in maintaining the overall health of both vaginal and urinary tissues, and as the level of this hormone decreases in menopause, the following changes can be noticed:
If you find that these approaches don’t provide relief, or if the dryness is significantly impacting your quality of life, don't stay quiet, it’s a good idea to consult a healthcare provider. They can offer personalised advice and explore additional treatment options.
Your vaginal health is an essential element of your overall well-being, particularly for women as they age and experience menopause.
By understanding what's normal and what's not, you can take the necessary steps to maintain good vaginal health, crucial not only for your physical comfort, but also for emotional and psychological well-being.
Perimenopause, the transition phase leading up to menopause, often brings a variety of changes to a woman's menstrual cycle
Bleeding In Between Periods & Perimenopause: Is it Normal?Tips on how to manage heavy bleeding during perimenopause.
Learn all about the causes, symptoms and treatments of bladder weakness during menopause.
Bladder Leaks During The Menopause
Yes, many women experience vaginal dryness due to decreased oestrogen, which can lead to discomfort during intercourse and increased risk of irritation or infections.
We advise visiting your doctor if you notice, thick or clumpy discharge (like cottage cheese). Yellow/Green frothy discharge with a strong odour. Grey or fishy smelling discharge, or excessive discharge with burning or irritation. All of these symptoms can indicate an infection may be present.
Yes, during perimenopause, many women who have not noticed discharge for years, may find it returns. Why because fluctuating oestrogen levels lead to changes in vaginal flora and create discharge. Some women experience more dryness, while others may notice increased or different types of discharge.
Vaginal discharge may decrease after menopause, but it usually doesn’t disappear completely. However, some women may still have some discharge after menopause, especially if they use hormone therapy or vaginal moisturisers.